Hyperhomocysteinemia is when homocysteine levels in the blood are too high, leading to health issues like recurrent pregnancy loss. This article explains what causes hyperhomocysteinemia, how it affects health, particularly in women, and the role of folic acid and vitamin B12 in managing it.
Key Takeaways
Hyperhomocysteinemia is linked to significant health risks, including cardiovascular diseases and recurrent pregnancy loss, particularly in women of reproductive age.
Folic acid and vitamin B12 play essential roles in managing homocysteine levels, and their adequate intake is vital for reducing adverse pregnancy outcomes.
Genetic factors, especially variations in the MTHFR gene, contribute to elevated homocysteine levels, highlighting the need for targeted interventions and screenings in at-risk individuals.
Understanding Hyperhomocysteinemia

Hyperhomocysteinemia, characterized by excessively high levels of homocysteine in the blood, is a condition with far-reaching implications for health. Elevated homocysteine levels can lead to a range of complications, from cardiovascular diseases to severe impacts on mental health and fertility. The metabolism of homocysteine is intricately linked with folate and vitamin B12, highlighting the importance of maintaining adequate levels of these nutrients.
In women, particularly those of reproductive age, high homocysteine levels can severely harm the nervous system, exacerbate mental health disorders, and increase the risk of cardiovascular diseases. Identifying the causes and impacts of hyperhomocysteinemia aids in creating effective prevention and treatment strategies.
Causes of Elevated Homocysteine Levels
The causes of elevated homocysteine levels are multifaceted, involving both genetic and environmental factors. Deficiencies in essential vitamins, particularly folate, vitamin B6, and vitamin B12, are significant contributors to hyperhomocysteinemia. These vitamins are crucial for the proper metabolism of homocysteine, and their absence can lead to its accumulation in the blood.
Genetic influences also play a pivotal role. Variations in genes responsible for homocysteine metabolism, such as the MTHFR gene, can predispose individuals to higher homocysteine levels. Additionally, lifestyle choices, including poor diet and lack of physical activity, further exacerbate the problem.
Recognizing these causes helps in addressing and managing hyperhomocysteinemia effectively.
Impact on Women’s Health
Elevated homocysteine levels pose significant risks to women’s health, particularly concerning cardiovascular diseases. This condition can harden and narrow the arteries, affecting coronary, cerebral, and peripheral blood vessels, thus increasing the risk of cardiovascular complications. For women, the implications are profound, as cardiovascular diseases remain a leading cause of mortality.
Moreover, hyperhomocysteinemia can exacerbate mental health disorders, including depression and dementia. Studies have shown that 20-30% of patients with both hyperhomocysteinemia and depression exhibit more severe symptoms, underlining the need for effective management of homocysteine levels to improve mental health outcomes.
This dual impact on physical and mental health makes hyperhomocysteinemia a critical area of concern for women’s health.
Hyperhomocysteinemia and Recurrent Pregnancy Loss

Recurrent pregnancy loss is a heartbreaking experience for many women, and emerging evidence points to hyperhomocysteinemia as a potential culprit. Elevated homocysteine levels during pregnancy have been linked to adverse outcomes, including recurrent early pregnancy loss and complications such as stillbirth and placental abruption. These findings suggest that managing homocysteine levels could be crucial for improving pregnancy outcomes.
Genetic factors, particularly mutations in the MTHFR gene, further complicate this issue. These genetic variations can lead to persistently high homocysteine levels, disrupting normal reproductive functions and increasing the likelihood of pregnancy loss. Grasping the mechanisms behind these associations is key to creating targeted interventions for at-risk women.
Mechanisms of Impact
The mechanisms by which elevated homocysteine levels impact pregnancy are complex and multifaceted. High homocysteine levels can cause capillary damage, negatively affecting the blood supply to the placenta. This damage can lead to placental insufficiency, which is a critical factor in pregnancy viability. The endometrial wall’s capillaries become less functional, disrupting the crucial exchange of nutrients between mother and fetus.
However, the relationship between hyperhomocysteinemia and intrauterine growth retardation (IUGR) remains somewhat ambiguous, with studies showing contradictory results. This inconsistency underscores the necessity for additional research to fully grasp the influence of elevated homocysteine levels on fetal growth and development.
Case Studies and Data
Significant associations between hyperhomocysteinemia and recurrent pregnancy loss have been documented through various studies. For instance, one study found that 32% of women with recurrent pregnancy loss had elevated homocysteine levels, while another reported that 33% of women experiencing secondary miscarriages had hyperhomocysteinemia. These findings underscore the potential role of homocysteine in pregnancy complications.
Despite the compelling data, only a few studies have systematically explored this relationship. Further research, including large prospective cohort studies and systematic reviews, is needed to establish a definitive link and develop effective prevention and treatment strategies for women at risk of recurrent pregnancy loss due to hyperhomocysteinemia.
Role of Folic Acid and Vitamin B12 in Managing Homocysteine Levels
Folic acid and vitamin B12 are crucial in managing homocysteine levels, particularly during pregnancy. These nutrients play vital roles in DNA synthesis and homocysteine metabolism, making their adequate intake essential for maternal and fetal health. Insufficient dietary intake of these vitamins can lead to elevated homocysteine levels, exacerbating pregnancy complications.
Managing homocysteine levels typically involves a blend of dietary, lifestyle, and medical strategies. Knowing the roles of folic acid and vitamin B12 is crucial for creating effective supplementation regimens for women at risk of hyperhomocysteinemia.
Importance of Folic Acid Supplementation
Folic acid supplementation is vital for preventing neural tube defects in newborns and managing homocysteine levels in pregnant women. Periconceptional intake of folic acid significantly reduces the risk of neural tube defects and supports healthy fetal development. Women with MTHFR mutations should ensure adequate folate concentrations to lower the risk of elevated homocysteine levels.
Vitamin B12 supplementation is equally important, especially for vegetarians and vegans who might not get enough from their diet. Folic acid and vitamin B12 together can help manage homocysteine levels effectively, reducing the risk of pregnancy complications.
Effects of Vitamin B12
Vitamin B12 is essential for proper homocysteine metabolism, playing a vital role in converting homocysteine back to methionine. This conversion is crucial for reducing homocysteine levels and supporting various metabolic processes. Adequate vitamin B12 intake is therefore essential for maternal health and fetal development.
Sources of vitamin B12 include meat, dairy products, and fortified foods. For those who may not consume enough of these foods, supplementation is recommended to ensure adequate intake and support healthy homocysteine metabolism.
Combined Supplementation Strategies
Combining folic acid and vitamin B12 supplementation strategies enhances the management of elevated homocysteine levels during pregnancy. This synergistic approach not only supports homocysteine metabolism but also optimizes maternal and fetal health outcomes. Medical professionals often recommend this combined supplementation to ensure comprehensive nutritional support for women at risk.
Recognizing genetic variants like the MTHFR gene helps in personalized nutritional management, boosting the effectiveness of supplementation strategies. Tailored approaches can significantly improve homocysteine management and pregnancy outcomes.
Genetic Factors and MTHFR Gene Mutation
Genetic variations, particularly in the MTHFR gene, play a significant role in hyperhomocysteinemia. These mutations can lead to higher homocysteine levels, increasing the risk of pregnancy complications and other health issues. The MTHFR C677T polymorphism is particularly notable for its association with lifelong elevated homocysteine levels.
Identifying genetic factors contributing to hyperhomocysteinemia is vital for creating targeted interventions and managing the condition effectively. Genetic screening can identify women at risk and inform personalized treatment strategies.
Screening for MTHFR Mutations
Screening for MTHFR mutations includes genetic tests to detect polymorphisms like C677T. PCR amplification is commonly used for this purpose, requiring a small blood sample collected through venipuncture. This screening is particularly important for women with unexplained sterility or recurrent pregnancy loss.
Fasting homocysteine levels are also assessed during the screening process to provide a comprehensive understanding of the individual’s risk profile. Detecting these genetic mutations can help guide interventions to manage homocysteine levels effectively.
Implications for Treatment
Recognizing the MTHFR gene mutation is essential for determining the right treatment for women with recurrent pregnancy loss linked to hyperhomocysteinemia. Tailored vitamin supplementation, including folic acid and vitamin B12, can effectively lower homocysteine levels and improve pregnancy outcomes.
Periconceptional folic acid supplementation not only lowers homocysteine levels but also reduces the risk of neural tube defects, supporting healthier pregnancies. Combining folic acid and vitamin B12 supplementation strategies can optimize homocysteine management and enhance maternal and fetal health.
Adverse Pregnancy Outcomes Linked to Hyperhomocysteinemia
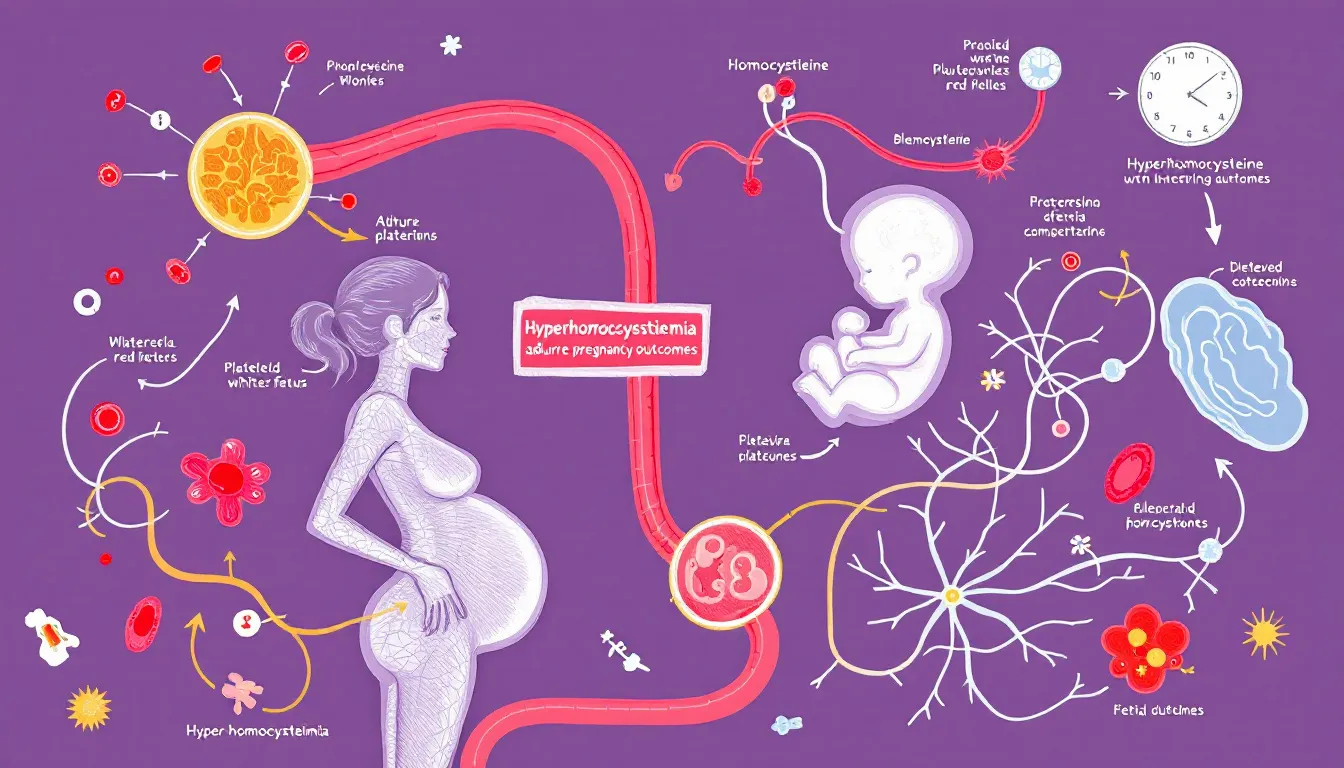
Hyperhomocysteinemia is linked to various adverse pregnancy outcomes, including:
deep vein thrombosis
abruption placentae
fetal growth restriction
These complications underscore the importance of managing homocysteine levels during pregnancy to ensure better maternal and fetal outcomes.
The connection between elevated homocysteine levels and conditions such as preeclampsia further highlights the need for effective management strategies. Preventing these adverse outcomes requires a comprehensive approach involving dietary, lifestyle, and medical interventions.
Preterm Birth and Low Birth Weight
Women with elevated homocysteine concentrations face a significantly higher risk of preterm births and low birth weight. Studies indicate that these women are at about twelve times greater risk of experiencing preterm births and nearly four times more likely to deliver low-birth-weight neonates. This association highlights the importance of managing homocysteine levels to ensure healthier pregnancy outcomes.
The increased likelihood of preterm births and low birth weight underscores the critical need for early pregnancy intervention and management strategies to support fetal growth and development.
Preeclampsia and Hypertensive Disorders
Preeclampsia and other hypertensive disorders of pregnancy are significant complications linked to hyperhomocysteinemia. Elevated homocysteine levels can negatively impact the vascular system, leading to increased blood pressure and vascular damage. This damage contributes to the development of preeclampsia, a condition characterized by high blood pressure and potential damage to organ systems.
The link between elevated homocysteine levels and preeclampsia highlights the importance of monitoring and managing these levels during pregnancy. Effective management can help mitigate these risks and support better pregnancy outcomes.
Placental Abruption and Stillbirth
Maternal hyperhomocysteinemia is associated with an increased risk of placental abruption, where the placenta detaches prematurely from the uterus, which can lead to stillbirth. Elevated homocysteine levels are considered a warning sign for potential placenta mediated complications during pregnancy.
This association highlights the critical need for early detection and management of elevated homocysteine levels to prevent such severe complications. Proactively addressing these risks can improve maternal and fetal outcomes and reduce stillbirth incidence.
Preventive Measures and Lifestyle Changes
Implementing preventive measures and lifestyle changes is crucial for managing high homocysteine levels and reducing the associated health risks. Maintaining healthy homocysteine levels is essential for overall health and particularly critical during pregnancy to prevent complications such as preeclampsia and recurrent pregnancy loss. By adopting specific dietary and lifestyle modifications, women can significantly reduce their risk factors.
Preventive strategies include dietary recommendations, lifestyle modifications, and medical interventions, forming a comprehensive approach to managing hyperhomocysteinemia and supporting better health outcomes.
Dietary Recommendations
Diet plays a pivotal role in managing homocysteine levels. Foods high in folate, such as dark green vegetables, legumes, and fortified cereals, are essential for maintaining healthy homocysteine metabolism. Including these foods in the diet can help manage homocysteine levels effectively, especially for women experiencing health complications related to pregnancy.
Additionally, incorporating vitamin B12-rich foods, such as meat, dairy products, and fortified foods, can further support healthy homocysteine metabolism. These dietary changes are crucial for managing homocysteine levels and ensuring better health outcomes.
Lifestyle Modifications
Regular physical activity is another important factor in managing homocysteine levels. Studies have shown that regular exercise can significantly help in reducing homocysteine levels. Engaging in physical activities not only supports cardiovascular health but also helps in maintaining optimal homocysteine levels.
Quitting smoking is equally crucial, as tobacco use can elevate homocysteine levels and negatively impact vascular health. Adopting these lifestyle changes can improve overall health and reduce risk factors related to hyperhomocysteinemia.
Medical Interventions
Routine monitoring and management of homocysteine levels are critical for pregnant women at risk of hyperhomocysteinemia. Working with a trained medical professional is crucial for developing a strategy to manage homocysteine levels effectively. Regular monitoring is crucial for individuals with a history of elevated homocysteine levels or cardiovascular diseases.
Healthcare providers can offer tailored interventions and adjustments to supplementation regimens to maintain optimal homocysteine levels during pregnancy. These interventions can significantly reduce the risk of complications and support better maternal and fetal outcomes.
Summary
In conclusion, managing hyperhomocysteinemia is crucial for improving pregnancy outcomes and overall health. Elevated homocysteine levels are linked to various complications, including recurrent pregnancy loss, preterm birth, preeclampsia, and placental abruption. Understanding the role of folic acid and vitamin B12 in homocysteine metabolism and the impact of genetic factors such as the MTHFR gene mutation is essential for developing effective prevention and treatment strategies.
By adopting dietary recommendations, lifestyle modifications, and medical interventions, women can significantly reduce their risk factors and support healthier pregnancies. Proactive management of homocysteine levels is key to ensuring better maternal and fetal outcomes, ultimately contributing to healthier families and communities.
Frequently Asked Questions
What is hyperhomocysteinemia?
Hyperhomocysteinemia is a condition defined by elevated homocysteine levels in the blood, which can increase the risk of cardiovascular diseases and complications in pregnancy. It is essential to monitor and manage homocysteine levels for overall health.
How does hyperhomocysteinemia affect pregnancy?
Hyperhomocysteinemia during pregnancy can lead to serious complications, including recurrent pregnancy loss, preterm birth, preeclampsia, and placental abruption. It is crucial to monitor and manage homocysteine levels to promote a healthy pregnancy.
What role do folic acid and vitamin B12 play in managing homocysteine levels?
Folic acid and vitamin B12 are crucial for the metabolism of homocysteine, and their supplementation effectively reduces homocysteine levels, thus preventing associated health complications.
What are the genetic factors involved in hyperhomocysteinemia?
Genetic variations in the MTHFR gene significantly contribute to hyperhomocysteinemia by influencing homocysteine metabolism. Screening for MTHFR mutations is essential for identifying individuals at risk and guiding treatment.
What lifestyle changes can help manage homocysteine levels?
To manage homocysteine levels effectively, it is crucial to engage in regular physical activity, quit smoking, and include foods rich in folate and vitamin B12 in your diet. These lifestyle changes can significantly reduce related health risks.

